Durotomy During Fronto-orbital Advancement: Harmful or Harmless?
Jessica Blum1, Daniel Y Cho1, Eric Winter2, Dillan Villavisanis1, Maria Punchak3, Scott P Bartlett1, Jordan W Swanson 1, Gregory G Heuer3, Shih-Shan Lang3, Phillip B Storm3, Jesse A Taylor1
1Division of Plastic, Reconstructive, and Oral Surgery, University of Pennsylvania and Children's Hospital of Philadelphia Philadelphia, PA; 2Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA; 3Division of Neurosurgery, Children's Hospital of Philadelphia, Philadelphia, PA
Background: Disruption of the dura mater during craniosynostosis repair can be unintentional, occurring during craniotomy, or intentional to directly measure intracranial pressure (ICP). This study aims to describe the outcomes of unintentional and intentional dural disruption in patients undergoing surgical repair of craniosynostosis.
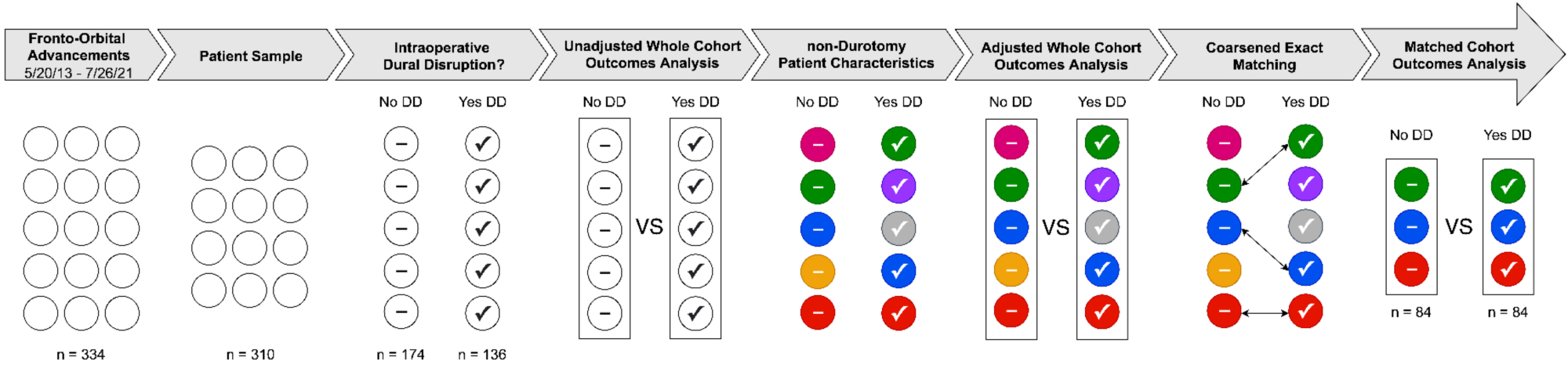
Methods: Patients who underwent their first bilateral fronto-orbital advancement (BFOAR) at our institution between 2013 and 2021 were included. Charts were retrospectively reviewed for demographic information, medical history, admission timeline, operative and anesthetic details, and complications. Analysis of the cohort was performed using multiple logistic regression. Additionally, a matched cohort was generated using coarsened exact matching (CEM), whereby patients were matched on the following factors: sex, race, age, affected suture(s), syndromic status, prior craniofacial surgery, and postoperative antibiotics (Figure 1). Complications were distinguished as perioperative or postoperative—occurring at least one-week post-discharge.Results310 patients were included in whole cohort analyses (136 with dural disruption, 174 without). Patients in the dural disruption group were significantly older than those without dural disruption (24.3% vs. 10.3% ? 5 years old, p<.001). There were no significant differences between cohorts for any other characteristics (p>.05).The most common perioperative finding was a transfusion requirement (n=9, 39%), followed by CSF leak (n=1, 4.4%).The most common postoperative complications were related to delayed wound healing (n=22, 44.0%). Infectious complications developed in (n=18) 5.8% of patients. Ten (55.6%) of these cases were related to the wound site, with five requiring operative intervention.Application of CEM yielded 84 matched cohorts, with 35 patients in the unintentional durotomy group and 74 in the ICP measurement group. The matched cohort had a comparable male, metopic, non-syndromic, 0–12-months-old majority (p>0.999 for all).Adjusted whole cohort analysis revealed intentional durotomy for ICP measurement as a protective factor for perioperative complications (OR=0.18, 95% CI:0.03–0.70, p=0.032). CEM similarly revealed ICP measurement as a protective factor for perioperative complications (OR = 0.125, 95% CI:0.01–0.93, p=0.039. Unintentional durotomy did not significantly increase the risk of perioperative, postoperative, or infectious complications (p>.05 for all).
Conclusions: Durotomies, intentional or unintentional, are not associated with an increased risk of complications in BFOAR. Intentional durotomy for ICP measurement was a protective factor for our cohort in matched and unmatched analyses. While causation cannot be gleaned due to methodology, this may be attributable to normalization of PCO2 to 35 mmHg for ICP measurement, lowering cerebral blood flow and intraoperative blood loss.
Back to 2022 Posters