Surgical management of vascular malformations of the upper extremity: an 11-year retrospective review of pediatric patients
Tessa Muss*, Sophia Hu, Mimi Kim, Yoshiko Toyoda, Emily Graham, Ines C. Lin
Division of Plastic Surgery, University of Pennsylvania, Philadelphia, PA
Vascular malformations (VMs) of the upper extremity (UE) are a heterogeneous group of lesions that can pose unique functional challenges. Surgery is one of the mainstays of treatment, but contemporary literature on surgical management of VMs is sparse. This retrospective study provides an update on the surgical management and outcomes of pediatric patients with UE VMs.
A retrospective review of patients evaluated at the Children's Hospital of Philadelphia between 2010-2021 was performed. Inclusion criteria: patients <18 with UE VMs who had surgery within the study period. Exclusion criterion: lack of operative management. Demographics, lesion characteristics, treatments, and outcomes were collected. ANOVA, chi-square, and Fisher's exact tests were used for data analysis.
A total of 34 patients and 43 operations were identified, with an average of 1.26 operations per patient and average age of 5.83 years. 64.7% of patients were White, 70.6% were male, and 64.7% had right-sided VMs. 47.1% of VMs were venous, 17.6% were unspecified, 14.7% were venolymphatic, and 8.8% were lymphatic. 38.2% of VMs were on the hand, 26.5% on the forearm, and 14.7% on the upper arm. The average VM diameter was 3.64 cm and 29.4% were associated with a functional deficit. All VMs were managed with direct surgical excision. 76.7% required subcutaneous excision and 20.9% required subfascial/intramuscular excision. 11.6% required neurolysis. 95.3% of excisions were closed primarily. There was a 7% complication rate and 16.2% of patients had recurrence requiring additional operations. 24 patients had at least 1 year of follow-up, of which 70.8% had no residual VMs, but 29.2% had persistent VMs despite treatment.
Surgery is a safe, effective option for localized, well-delineated UE VMs and can be used to achieve primary closure on lesions with relatively low complication rates. It may be utilized more often in subcutaneous locations over deeper involvement. In line with other literature, recurrence is fairly common, and a proportion of patients may continue to have residual VMs despite treatment.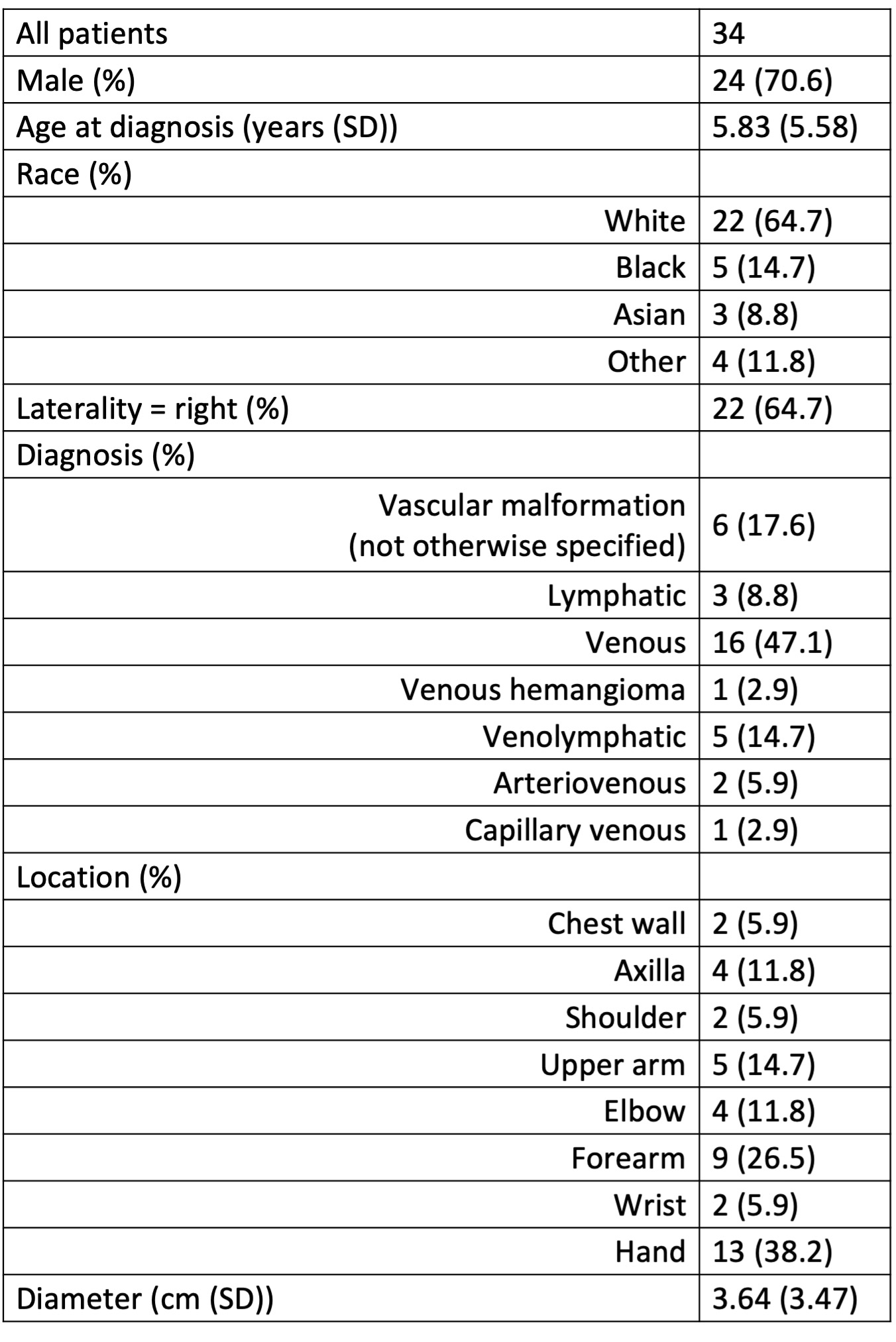
Table 1. Demographics and lesion characteristics of UE VMs.
Back to 2023 Abstracts


