Limb-itless Possibilities: Management of Osseointegrated Implant Infections and Explantations in Lower Limb Amputees
Grant G. Black*1, Anna M. Vaeth1, Yunchan Chen1, Albert Truong1, Taylor J. Reif3, S. R. Rozbruch3, Michael W. Henry2, David Otterburn1
1Plastic and Reconstructive Surgery, Weill Cornell Medicine, New York, NY; 2Infectious Diseases, Hospital for Special Surgery, New York, NY; 3Limb Lengthening and Complex Reconstruction, Hospital for Special Surgery, New York, NY
Osseointegrated implants (OI), an alternative to traditional socket-suspended prostheses for lower limb amputees, eliminate the socket-skin interface and allow for weight-bearing directly on the skeletal system. However, the stoma through which the implant attaches to the external prosthesis creates an ingress route for bacteria, and infection rates as high as 66% have been reported. The aims of this study are to classify infection management and long-term outcomes in this patient population.
A retrospective analysis was performed on all patients who received lower limb OI at our institution between 2017 and 2022. Demographic, operative, and outcome data were collected for all patients. Patients were stratified by the presence and severity of infection. Chi-squared and t-tests were performed on categorical and continuous data, respectively, using an alpha of 0.05.
102 patients met our study criteria; 62 had transfemoral OI and 40 had transtibial OI. Patients were followed for 23.8 months on average (range: 3.5-60.3). There were a total of 31 superficial stoma infections, 15 deep soft tissue infections, and 7 cases of osteomyelitis. All stoma infections resolved after 13±7 days of topical or oral antibiotics. All deep soft tissue infections were treated with 33±28 days of systemic antibiotics, and 2 (13%) required operative washout. Osteomyelitis was managed with 81±69 days of systemic antibiotics. All cases received operative attention, including 5 (71%) washouts and 2 (29%) explantations. Both implants were replaced 3.5 months after explantation. There was no correlation between history of soft tissue infection and development of osteomyelitis (p>0.05). The overall implant salvage rate after infection was 96%.
This study describes our institution's experience managing infection after OI and soft tissue reconstruction. Although infections do occur, they are easily treatable and rarely require operative intervention. Explantation due to infection is uncommon and can be followed up with reimplantation, reaffirming that OI is a safe and effective treatment modality.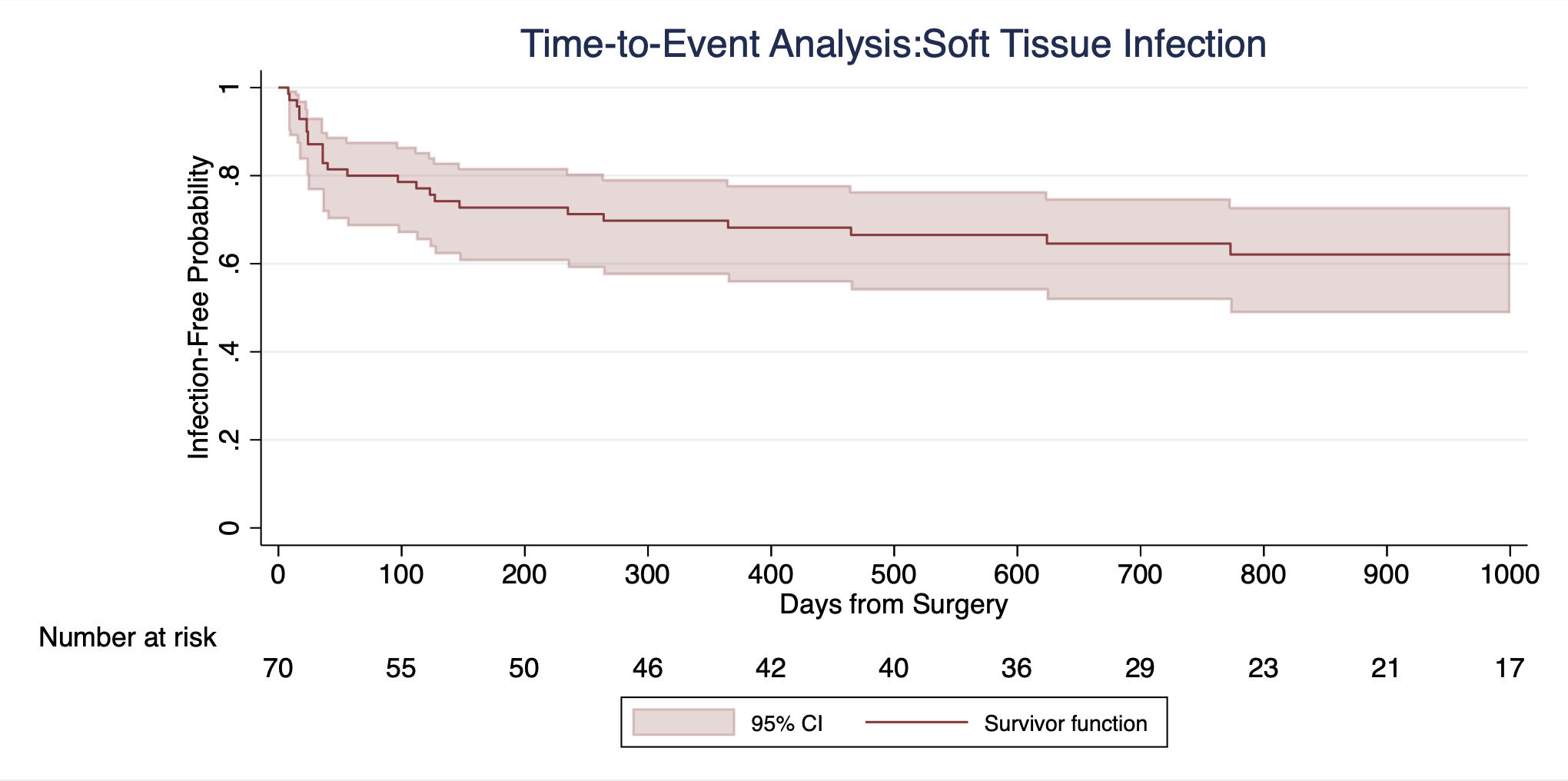
Time to event analysis of soft tissue infections after osseointegrated implantation shows that 47% of infections develop in the first month after implantation, and 76% develop in the first 3 months after implantation.
Back to 2023 Abstracts


