Alternative Patterns of Superficial Lymphatic Drainage in the Breast and Trunk after Breast Cancer Surgery
Meeti Mehta*1, Elizabeth A. Moroni2, Carolyn De La Cruz2
1Department of Plastic Surgery, University of Pittsburgh School of Medicine, Pittsburgh, PA; 2Department of Plastic Surgery, University of Pittsburgh, Pittsburgh, PA
Changes in superficial lymphatic drainage from the chest wall/trunk after breast cancer treatment are not well described. This study examines alternative lymphatic flow in the post-mastectomy lymphedema population to identify risks associated with truncal and upper extremity lymphedema.
Patients undergoing revision breast surgery with suspicion of lymphedema from 2014-2020 were offered lymphangiography. Breasts and trunks were visualized and blindly evaluated for alternative drainage. Summary statistics were computed, and linear Cohen's Kappa statistic was used to compare rater agreement. Binomial regression was used to compute relative risks (RR).
86 sides (46 patients) were included. 12 sides underwent no treatment and were considered controls. 88% of the non-controls had alternative lymphatic flow. This was seen in ipsilateral axillae (64%), ipsilateral groins (57%), contralateral axillae (20.3%), and contralateral groins (9.3%). Cohen's Kappa for alternative drainage was 0.631 ± 0.043. Ipsilateral axillary and contralateral inguinal drainage reduced risk of truncal lymphedema (RR 0.78, CI 0.63-0.97, p=0.04; RR 0.32, CI 0.13-0.79, p=0.01, respectively). Radiation therapy increased risk of truncal and upper extremity lymphedema (RR 3.69, CI 0.96-14.15, p=0.02; RR 1.92, CI 1.09-3.39, p=0.03, respectively). Contralateral axillary drainage and axillary lymph node dissection increased risk of upper extremity lymphedema (RR 4.25, CI 1.09-16.61, p=0.01; RR 2.83, CI 1.23-6.52, p=0.01, respectively).
This study highlights several risk/protective factors for truncal and upper extremity lymphedema. Ipsilateral axillary and contralateral inguinal drainage are protective against truncal lymphedema. Patients with radiation, axillary lymph node dissection and contralateral axillary drainage are at highest risk of upper extremity lymphedema.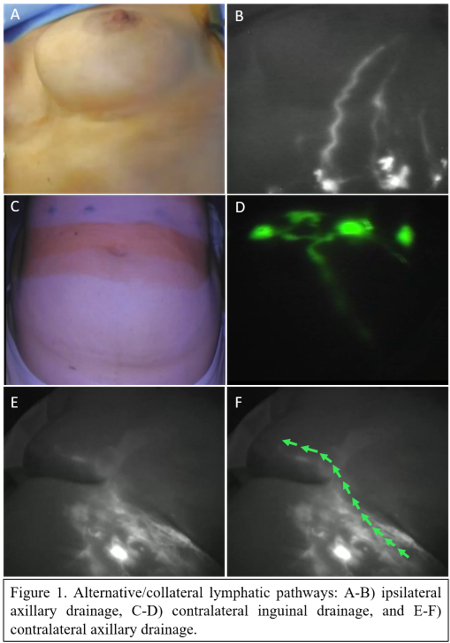
Back to 2023 Abstracts


