The Effect of Obesity on Vaginoplasty Outcomes
Lauren E. Berger*1, Daisy L. Spoer1, Samuel S. Huffman1, Christian X. Lava2, Taylor Martin2, Jenny C. Bekeny1, Kenneth L. Fan1, David M. Lisle3, Gabriel A. Del Corral4
1Plastic and Reconstructive Surgery, MedStar Georgetown University Hospital, Washington, ; 2Georgetown University School of Medicine, Washington, ; 3Colorectal Surgery, Franklin Square Medical Center, Washington, ; 4Plastic and Reconstructive Surgery, Washington Hospital Center, Washington,
Background: Genital surgery, such as vaginoplasty, is an often important step in the gender affirmation process. However, some surgeons employ body mass index criteria within the patient selection processes, thereby limiting access to some obese patients. We sought to better characterize the effect of obesity on postoperative outcomes and revision rates across multiple vaginoplasty techniques.
Methods: A single-center retrospective review of all transfeminine patients undergoing primary vaginoplasty procedures from December 2018 to July 2022 was conducted. Patients were stratified into cohorts according to the World Health Organization Obesity Class criteria. Data regarding demographics, comorbidities, operative details, postoperative complications, and all-cause revision were collected and compared between cohorts.
Results: A total of 237 patients met inclusion criteria. Multivariate regression analysis revealed patients with class I and class II/III obesity were associated with significantly higher odds of developing vaginal stenosis (class I: OR 7.1, p=0.003; class II/III: OR 3.4, p=0.018). Further, obesity class I and II/III were predictors of all-cause revision (class I: OR 3.7, p=0.021; class II/III: OR 4.8, p=0.027). Undergoing either robotic peritoneal or robotic intestinal vaginoplasty was associated with lower odds of delayed wound healing (peritoneal: OR 0.2 95%, p<0.001; intestinal: OR 0.2, p=0.011). Lastly, adherence to dilation regimen was negatively associated with development of vaginal stenosis (OR 0.04, p<0.001) (Table 5).
Conclusion: Patients with obesity may be at a higher risk of developing vaginal stenosis after vaginoplasty, which may ultimately necessitate operative revision. While patients with obesity may remain candidates for vaginoplasty, proper adherence to postoperative vaginal dilation regimens is critical to optimizing outcomes. Further, robotic approaches may prove an optimal alternative in this patient population, necessitating sufficient preoperative counseling.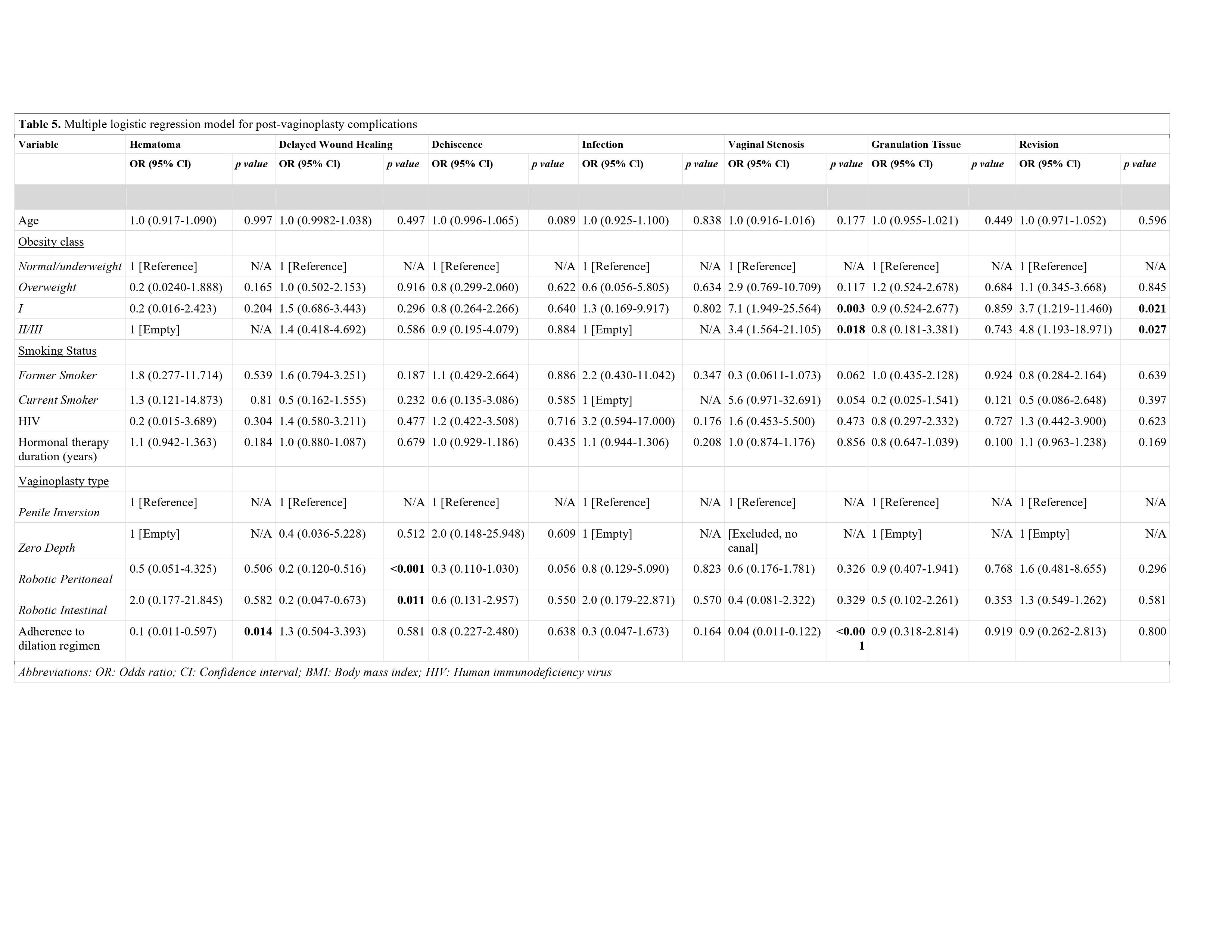
Table 5. Multiple logistic regression model for post-vaginoplasty complications.
Back to 2023 Abstracts


