Improved post-surgical satisfaction following primary vaginoplasty: associations with neovaginal canal width and introitus depth
Janet Coleman-Belin1, Subha Karim2, Anya Wang1, Shravya Gurrapu3, Dan Kahan4, Keren Cohen2, Ann Tran2, Bella Avanessian1, Elan Horesh1, John H. Pang2, Peter J. Taub1, Jess Ting1
1Plastic and Reconstructive Surgery, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Center for Transgender Medicine and Surgery, New York, NY; 3Columbia Vagelos College of Physicians and Surgeons, New York, NY; 4Albert Einstein College of Medicine, Bronx, NY
Dilator use following vaginoplasty maintains neovaginal patency and prevents neovaginal stenosis. While postoperative dilating practices are associated with improved post-surgical outcomes and satisfaction, there is limited evidence examining the extent of benefit offered by increased neovaginal canal depth and width.
The present study included 426 total postoperative visits of 197 unique patients who underwent primary vaginoplasty with the Mount Sinai Center for Transgender Medicine and Surgery (CTMS), had their first postoperative follow-up visit between 10/31/2017-9/3/2020, and reported introitus depth. Preoperative and postoperative Gender Dysphoria Index (GDI) (defined as patient-reported gender dysphoria on a 0-10 Likert scale, where 10 is maximum gender dysphoria), neovaginal canal width (in dilator color), and introitus canal depth (in dilator dot) were analyzed. Data were stratified into four groups by days following vaginoplasty and analyzed using linear regression.
Mean preoperative GDI was 5.77 (±2.82), mean postoperative GDI was 2.76 (±2.20); reduction in GDI following vaginoplasty was significant (p<0.001). There was no statistically significant association between neovaginal canal depth and GDI reduction across any time point ([0-30 days] p=0.956; [31-90] p=0.248; [91-180] p=0.573; [181-365] p=0.682). Neovaginal canal width at one month and six month postoperative visit time points revealed a weak negative correlation ([0-30] r= -0.0433, p=0.0046; [91-180] r= -0.0121, p=0.03) and may be incidental. Width did not reveal significant correlation with GDI reduction at three month and one year follow-up following primary vaginoplasty ([31-90] p=0.603; [181-365] p=0.605).
Primary vaginoplasty significantly reduced GDI among CTMS patients. Across all postoperative visit time points, neovaginal introitus depth and canal width were not meaningfully associated with GDI reduction. While it is highly likely that undergoing vaginoplasty improves patient quality of life, rapidly maximizing neovaginal canal depth and width postoperatively may not be as substantial.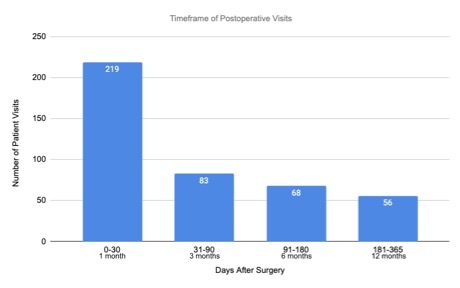
Figure 1. Postoperative visit frequency following vaginoplasty at time points: one month [0-30 days], three months [31-90 days], six months [91-180 days], and one year [181-365 days].
Back to 2023 Abstracts


