Quality of life outcomes after salvage laryngectomy studied in a survivorship program: microvascular free skin flaps vs pectoralis major myocutaneous flaps (PMMF)
Zainab Balogun1, Joseph W. Mocharnuk*1, Sophia Dang2, Marci Nilsen2, Jonas Johnson2, Seungwon Kim2, Umamaheswar Duvvuri2, Shaum Sridharan2, Mario G. Solari3, Mark Kubik2
1School of Medicine, University of Pittsburgh, Pittsburgh, PA; 2Department of Otolaryngology, University of Pittsburgh, School of Medicine, Pittsburgh, PA; 3Department of Plastic Surgery, University of Pittsburgh School of Medicine, Pittsburgh, PA
Salvage total laryngectomies or laryngopharyngectomies are usually followed by reconstruction to reestablish the continuity of the upper aerodigestive track, while also preserving function (speech and deglutition). The two most common reconstructive techniques include the pectoralis major myocutaneous flap (PMMF) and vascularized free flaps. The objective of this study was to evaluate the health-related quality of life outcomes related to the prevalence of chronic pain, dysphagia, and neck disability amongst patients who underwent free flap vs. pectoralis major myocutaneous flaps (PMMF) for reconstruction after salvage laryngectomy.
A retrospective chart review was conducted from a prospectively collected multidisciplinary head and neck cancer (HNC) Survivorship database. Patients with at least 6 months of post-operative follow-up from salvage total laryngectomy/total laryngectomies with partial pharyngectomies with subsequent free flap or pectoralis flap were included. Patients who underwent total laryngo-pharyngectomies were excluded. Primary outcome measures were validated patient-reported outcome measures (PROMs) including Functional Oral Intake Scale (FOIS), Eating Assessment Tool-10 (EAT-10), measure of chronic pain, shoulder mobility, and swallowing-specific University of Washington Quality of Life (UW-QOL) subscale scores and Neck Disability Index (NDI).
24 patients underwent pectoralis major myocutaneous flaps, and 30 patients underwent microvascular free flaps. Mean EAT10, chronic pain, shoulder mobility, and swallowing-specific University of Washington Quality of Life (UW-QOL) subscale scores, and Neck Disability Index (NDI) were not significantly different in these two groups. The mean FOIS was higher in patients reconstructed with pectoralis flaps (5.67 +/- 1.52 vs 4.57 +/- 2.12), p<0.05), but the clinical relevance of this is unclear.
In this study of salvage laryngectomy patients in a survivorship dataset, quality of life outcomes did not vary based on the type of vascularized tissue reconstruction (free flaps vs pectoralis flaps).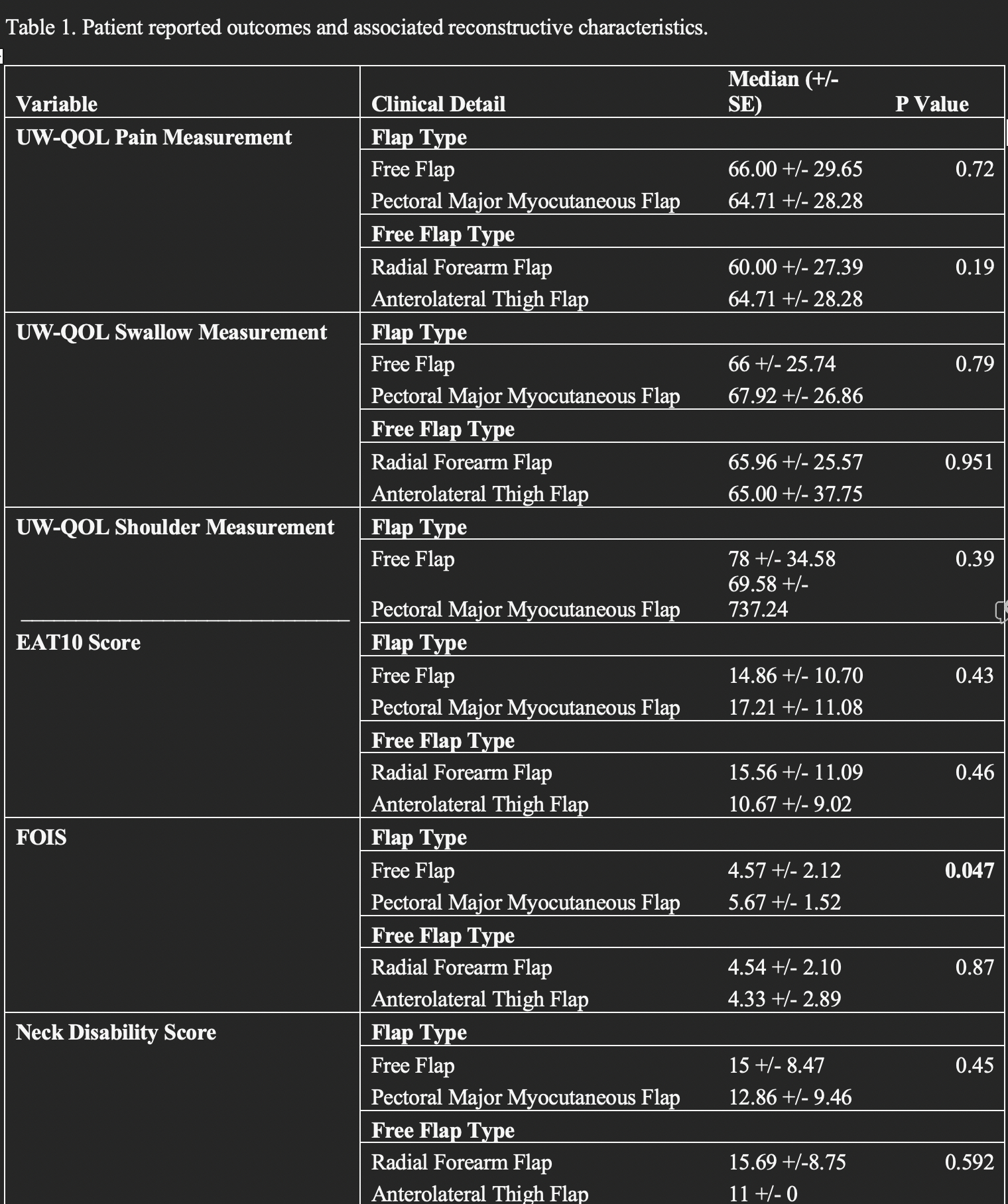
Table 1. Patient-reported outcomes and associated reconstructive characteristics.
Back to 2023 Abstracts


