Clinical Management of the Infected Tissue Expander: Assessing Salvage and Factors Associated with Successful Reconstruction
Perri S. Vingan*, Jonas Nelson, Francis Graziano, Max Mandelbaum, Danielle Rochlin, Julia Gutierrez, Kathryn Haglich, Michelle Coriddi
Plastic Surgery, Memorial Sloan Kettering Cancer Center, New York, NY
We aimed to examine our institutional salvage rate for infected tissue expanders (TE) and assess variables associated with reconstructive loss in managed cases of infection following immediate breast reconstruction.
Patients who underwent TE reconstruction following mastectomy from 2017 to 2022 were examined. Patients who had clinical signs or symptoms of infection within 1 year of TE placement were identified for analysis. 5 management cohorts were utilized: 1) intravenous (IV) antibiotics 2) interventional radiology (IR) drainage 3) TE removal and replacement with a new TE 4) TE removal and replacement with an implant 5) TE removal without replacement. Patients treated with oral antibiotics alone were excluded. Patients were followed for 1 year to assess their outcome following infection. Reconstructive failure was defined as device removal within 1 year of placement.
4619 patients had TEs placed, of which 311 (6.7%) had an infection meeting inclusion criterion: Factors significantly associated with infection on univariate analysis included age, BMI, hypertension (HTN), diabetes, radiation, reconstruction timing, ADM, TE plane, and mastectomy weight. On multivariable analysis, age, BMI, HTN, adjuvant radiation, bilateral TEs and ADM were associated with higher odds of infection, however TE pocket and neoadjuvant radiation did not significantly increase the odds of infection. There was a 54% failure rate within 1 year. Univariate analysis showed that race, infection management cohort, and cultured bacteria were associated with failed reconstruction. Patients with gram negative organisms in their cultures had high failure rates.
Infection following TE-based breast reconstruction is challenging, though nearly 50% of reconstructions were salvaged with focused management. All patients with infected TEs should be started on early IV antibiotics and the decision to bring to the OR should be based on clinical improvement with IV antibiotics. We no longer utilized IR drain placement and instead choose operative washout in cases of periprosthetic infected fluid collections.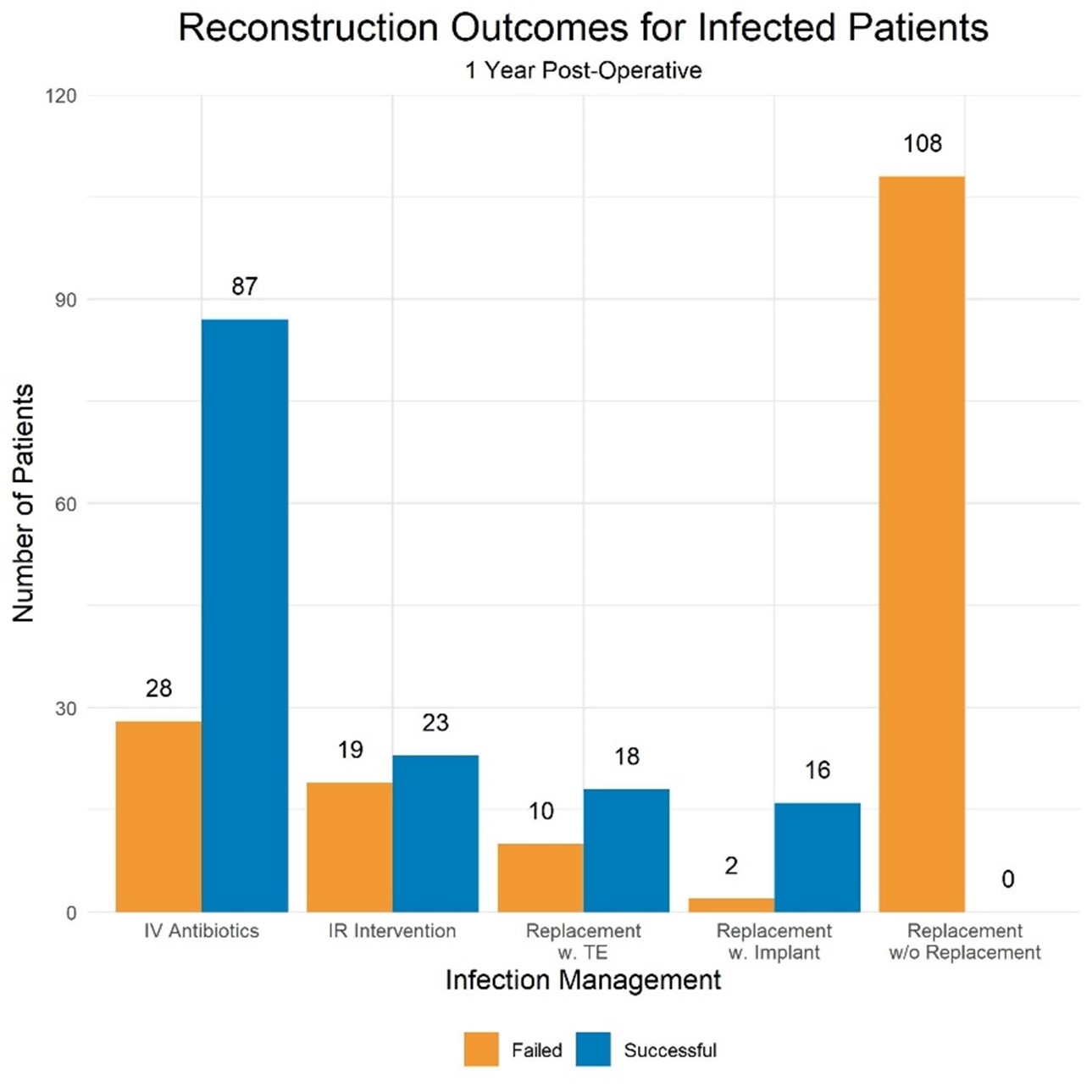
Back to 2023 Abstracts


