Catching the Catastrophic: A 10-Year NSQIP Analysis of Microsurgical Complications
Sarah Diaddigo*, Myles N. LaValley, Albert Y. Truong, David Otterburn
Columbia University, New York, NY
While surgical outcomes of microvascular free tissue transfer have been studied extensively, there is an absence of literature regarding the risk of medical catastrophes such as stroke, cardiac arrest, and pulmonary embolism. Despite significant advancements in the field, an outdated review of catastrophic medical outcomes (CMO) between 2006-2011 remains the benchmark for patient counseling and medical decision making. This study aims to provide an updated analysis of CMO in patients undergoing microvascular free tissue transfer by using a larger, more diverse cohort to inform guidelines of care.
This study uses data from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP). Cases of microvascular free tissue transfer from 2012-2021 were analyzed to assess the 30-day rates of CMO, defined as pulmonary embolism, respiratory failure, cardiac arrest, myocardial infarction, septic shock, coma, and death, and their associated risk factors. Demographic, comorbidity, and operative variables that differed significantly between patients with and without CMO were included in a binomial logistic regression.
Of the 22,839 included cases (62.3% breast, 27.4% head and neck, 2.9% extremity, and 7.4% other), 3.4% of patients experienced at least one CMO, including 99 deaths (0.4% mortality rate). CMOs occurred in 9.1% of head and neck reconstructions, compared to 1.4% of extremity and 0.9% of breast cases (p<0.001). The most common CMO was respiratory failure (2.3%) followed by pulmonary embolism (0.6%). Independent risk factors for CMO are shown in Table 1. CMOs were associated with an average 10-day delay in hospital discharge.
Compared to a previous study of the period between 2006-2011, the rate of CMOs decreased from 5.2% to 3.4%, but 30-day mortality rose slightly from 0.3% to 0.4%. Further research is needed to identify factors contributing to these changes in order to optimize patient outcomes, minimize complications, and reduce costs associated with microvascular free tissue transfer.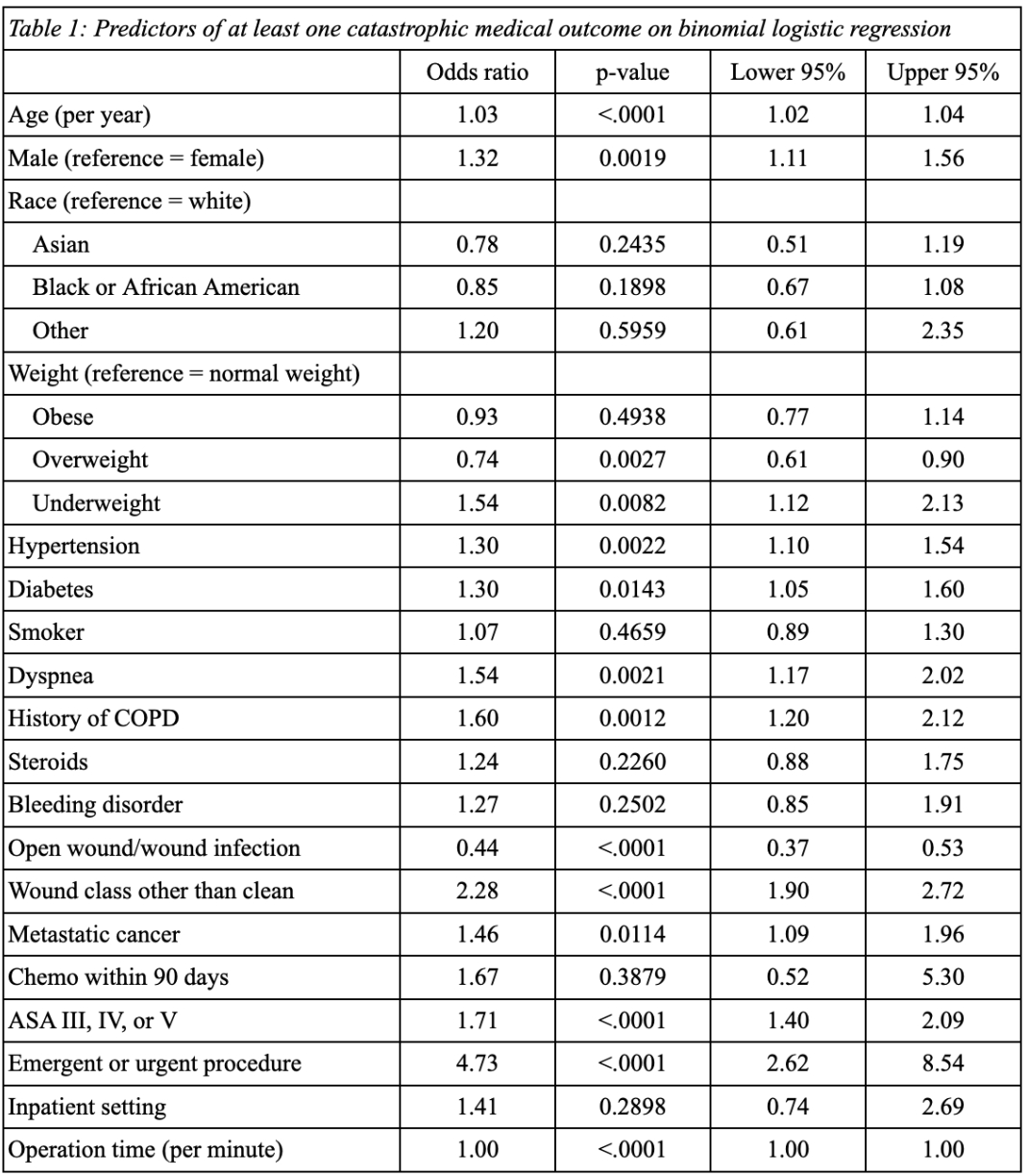
Back to 2023 Abstracts


