Refining Indications for Orbital Floor Exploration in Zygomaticomaxillary Complex Fractures
Luke Soliman*, Ben Rhee, Marina Hahn, Thor S. Stead, Rachna Goli, Nikhil Sobti, Damon McIntire, Vinay Rao, Albert Woo
Division of Plastic and Reconstructive Surgery, Warren Alpert Medical School of Brown University, Providence, RI
Guidelines for orbital floor exploration in the setting of zygomaticomaxillary complex (ZMC) fractures remain controversial. In this study, we aim to refine indications for orbital floor exploration by identifying clinical and radiographic parameters portending need for intervention.
A retrospective review was performed of patients with ZMC fractures evaluated by the plastic surgery department at a tertiary academic medical center. Patient demographic and clinical data were recorded. Preoperative computed tomography (CT) imaging was examined for radiographic parameters of interest. Patients were stratified into those receiving and not receiving orbital floor reconstruction. Receiver operating characteristic curves were calculated with sensitivity, specificity, and area under the curve (C-statistic) to predict patients not needing floor repair. A decision tree was formulated utilizing a naïve Bayes estimate to guide operative decision making.
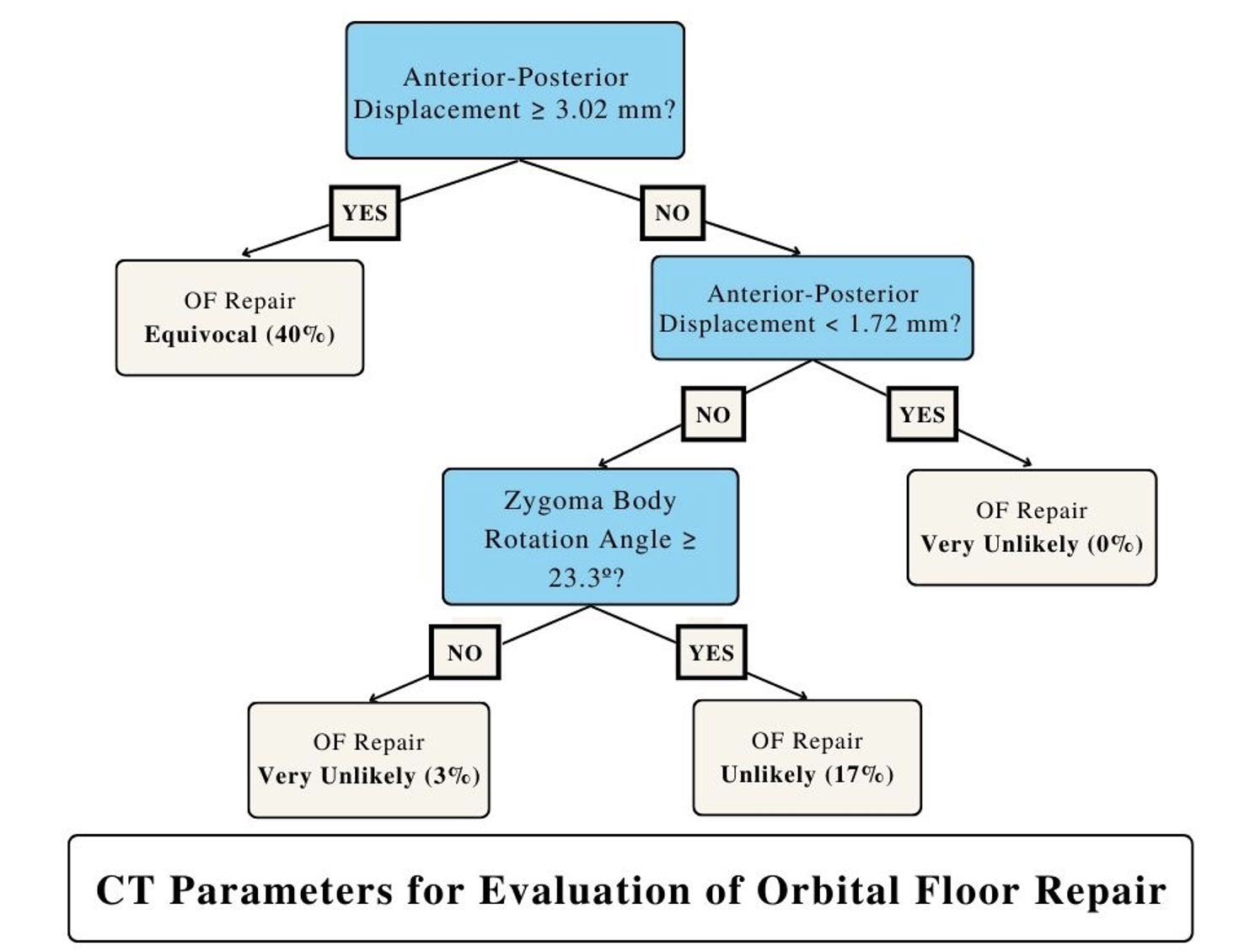
Of 232 patients with ZMC fractures, 14 (6.0%) underwent orbital floor exploration and repair. Concomitant nasoorbitoethmoid (p < 0.001, OR 4.36), LeFort (p = 0.003, OR 4.06), or medial orbital wall (p < 0.0001, OR 5.19) fracture portended need for floor repair. Radiographically, fractures requiring floor reconstruction demonstrated significantly increased posterior displacement of the zygoma (p = 0.0048). A nominal logistic regression model including age, zygoma rotation angle, and anterior-posterior demonstrated sensitivity, specificity, and C-statistic of 85.7%, 81%, and 0.9345, respectively (Figure 1). Below 1.72 mm of posterior zygomatic displacement, 0% of patients required floor repair (Figure 2).
Our nominal logistic regression model including features such as zygoma rotation and anterior-posterior displacement predicted the absence of need for floor exploration and repair in 93.5% of patients. Further, our model suggests that few patients with A-P displacement < 1.72 mm require floor repair. We believe these findings will serve to better delineate operative management for patients presenting with these injuries.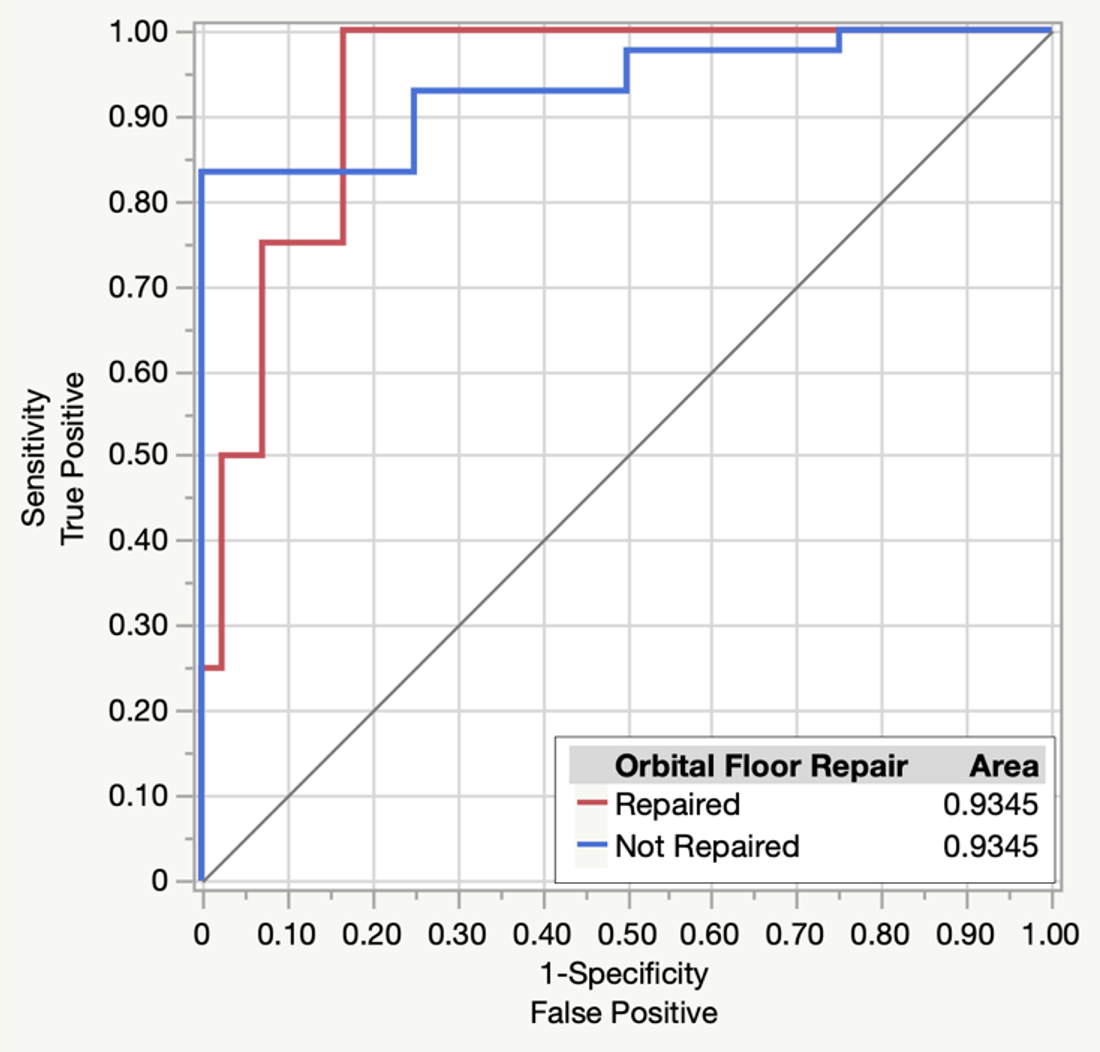
Back to 2023 Abstracts


