Risk Factors of Traumatic Brain Injury in Patients with Mandibular Fractures
Seray Er*1, Bashar Hassan2, Eric Resnick1, Allison Karwoski1, Judy Pan2, Fan Liang3, Michael Grant2
1University of Maryland School of Medicine, Baltimore, MD; 2Division of Plastic and Reconstructive Surgery, R. Adams Cowley Shock Trauma Center, University of Maryland Medical Center,, Baltimore, MD; 3Department of Plastic and Reconstructive Surgery, Johns Hopkins Hospital, Baltimore, MD
TBI associated with facial fractures is a major public health concern worldwide. Mild TBI has been reported in up to 38.4% of mandibular fractures, but risk factors of TBI in patients with mandibular fractures remain unknown. Our study is the first to evaluate these risk factors.
We retrospectively reviewed patients who presented with traumatic mandibular fractures in 2018 and 2019. Excluded were patients with no documentation of Glasgow Coma Scale (GCS) or neurologic symptoms/signs on presentation. Our primary outcome was prevalence of concomitant TBI on presentation defined as having GCS<15 or any neurologic symptom/sign. Persistent/incident post-traumatic neurologic symptoms were assessed at >4 weeks after injury. Bivariate analysis and multivariate logistic regression were performed.
Of n=220 patients, n=105 (47.7%) had concomitant TBI on presentation. Compared to patients with no TBI, patients with TBI were more likely to be older (mean age [standard deviation (SD)] 34.9 [15.1], 39.2 [16.5] years; P=.043), Non-Hispanic White (n=33 [28.7%], n=44 [42.3%]; P=.033) and have subcondylar fractures (n=14 [12.2%], n=25 [23.8%]; P=.033). Among covariates including fracture location and displacement, only subcondylar fractures had significantly increased odds (adjusted odds ratio [aOR] [95% confidence interval (CI)] 2.5 [1.1-5.6]) of TBI on presentation compared to fractures not involving the subcondyle. Of n=88 patients who were followed up for a median (interquartile range [IQR]) of 68.5 (43.3-147.3) days, n=51 (58.0%) had neurologic symptoms at >4 weeks following injury. Among covariates including fracture location and displacement, only fractures with >4 mm displacement had significantly increased odds (aOR [95% CI] 2.5 [1.1-25.5]) of having neurologic symptoms at >4 weeks after injury compared to fractures with <2 mm displacement.
Patients with subcondylar fractures and fractures with >4 mm displacement may benefit from TBI screening as well as a close and prolonged follow-up for persistent/incident neurologic symptoms.
P31
Time From Onset of Occipital Neuralgia Symptoms to Nerve Decompression Surgery
Merel H. Hazewinkel*1, Grant G. Black1, Katya Remy2, Sierra Tseng2, PG Matthew3, William G. Austen2, Lisa Gfrerer1
1Division of Plastic & Reconstructive surgery, Weill Cornell Medicine, New york city, NY; 2Harvard Medical School, Department of Plastic Surgery, Hand Surgery, and Peripheral Nerve Surgery, Boston, MA; 3Mass General Brigham Health, Department of Neurology, Foxborough, MA
In clinical practice, nerve decompression surgery is not routinely considered as part of the management algorithm for occipital neuralgia (ON). The aim of this study is to evaluate the time between onset of ON symptoms and nerve decompression surgery.
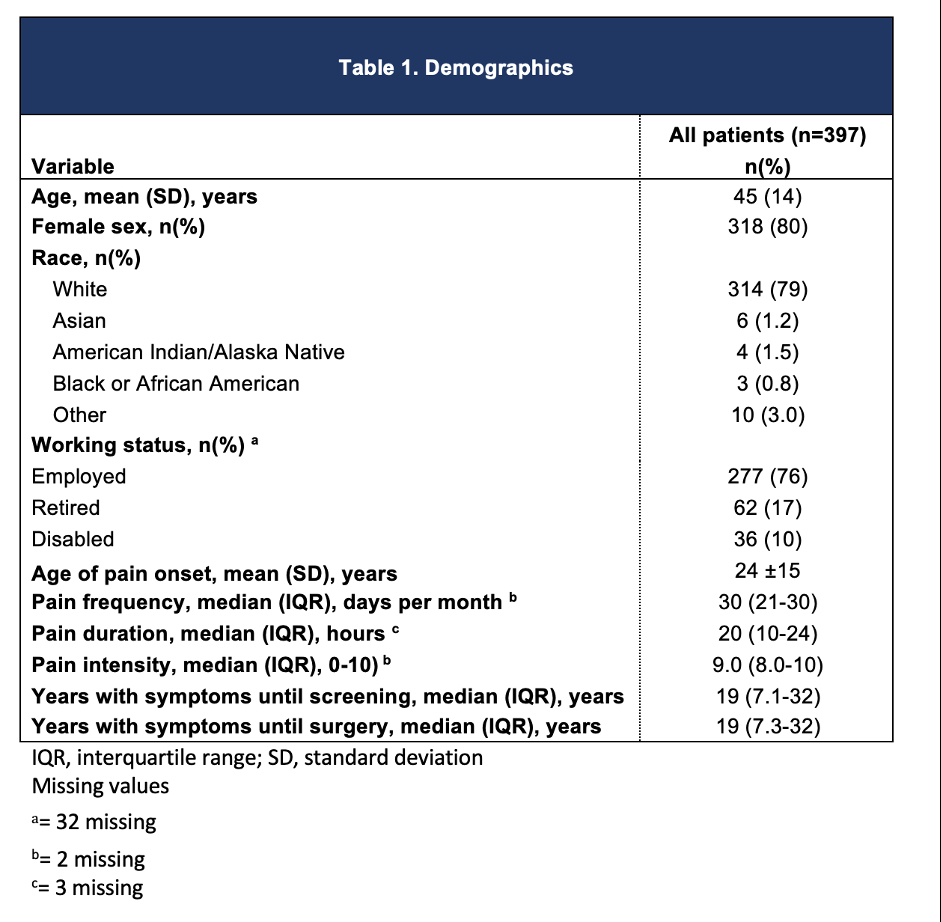
Patients that were screened for pericranial nerve decompression surgery between September 2012 and November 2022 were prospectively enrolled. Patients with a diagnosis of ON were included. Among the patients whom underwent ON decompression surgery, pain frequency (pain days per month), -intensity (scale of 0-10), and duration (in hours) were recorded preoperatively and at 12 months post-operatively.
397 patients met the inclusion criteria. Patients were predominantly female (80%). The average age of pain onset was 24 (±15) years. After screening, 158 (40%) patients underwent occipital nerve decompression. The average time between onset of ON symptoms and nerve decompression surgery was 19 years (7.3-32). The average time of postoperative follow-up was 8.9 (± 4.2) months. Among the patients that underwent surgery, the median number of pain days per month decreased from 30 (25-30) preoperatively to 8.0 (0-30) (73%) (p<0.001) post-operatively, the median pain intensity decreased from 9.0 (8.0-10.0) preoperatively to 5.0 (0-7.0) (44%) (p<0.001) post-operatively and the median pain duration in hours decreased from 24 (10-24) preoperatively to 4.0 (0-12) (83%) (p<0.001) post-operatively.
The results of this study demonstrate that patients experience ON for an average of 19 years prior to undergoing nerve decompression surgery. Occipital nerve decompression significantly improves pain frequency, duration and pain in patients experiencing ON and should be considered earlier in the treatment course of patients with refractory ON.
Back to 2023 Posters


